Episode #214: Strengthening Yourself with Helpful Facts About Menopause
Menopause: you had questions, we got you answers! In this riveting conversation with Amy’s gynecologist, Nurse Practitioner Julie Keeler, you’ll hear the medical/physical side of menopause. Julie helps us better understand our body’s changes, navigate a heightened set of emotions, address sleep disturbances, and more. Women of all ages will appreciate the real talk on an often-ignored topic!
(This page contains affiliate links. Your clicks and purchases help support Grit 'n' Grace at no extra charge to you.)
Recommended Resources
- Episode #208: Bursting Out of the First-Half-of-Life Boxes
Downloads
Your Turn
- In what phase do you find yourself? The reproductive years? Perimenopause? Post-menopause?
- What piece of information in today’s episode was new to you? How could this piece of information serve to improve your life?
- Where does physical self-care rank in your list of spiritual disciplines? Is this a healthy place for it to rank or do you need to prioritize it more?
Featured Guest — Julie Keeler
Julie has been a provider of women’s healthcare for over 3 decades. She is originally from Washington State where she earned her Bachelors of Science Degree in Nursing. For thirteen years following her graduation, she worked as a Registered Nurse in Labor and Delivery. While still living in Southern California, she also had the opportunity to receive her Nurse Practitioner education and earn a Master’s Degree in Nursing.
In 1996, Julie relocated with her family to the Raleigh area and worked initially as a Clinical Nurse Specialist and then in private practice as a Nurse Practitioner providing obstetric and gynecologic care. In early 2005, Julie had the good fortune to start a local women’s health practice which was a wonderful success.
Julie also has two terrific adult children, Sheridan and Bryce. When she has time, Julie enjoys the mountains, the beaches, quilting, landscaping, her dogs, chickens and kayaking!
Transcript — scroll to read here (or download above)
****
Grit ‘n’ Grace — The Podcast
Episode #214: Strengthening Yourself with Helpful Facts About Menopause
Amy Carroll 00:00
Today we are making good on a promise that we made last season
Cheri Gregory 00:04
after our episodes on the spiritual and emotional aspects of menopause. We promised to bring on a special guest to answer your questions on the physical aspects of menopause. Today,
Amy Carroll 00:16
we’re going to answer all your questions and I do mean also, you might want your earbuds in if they’re a little people in the room.
Cheri Gregory 00:24
Well, this is Cheri Gregory.
Amy Carroll 00:27
And I’m Amy Carol,
Cheri Gregory 00:28
and you’re listening to grit and grace, the podcast that equips you to lose so you’re not love who you are, and live your one life well.
Amy Carroll 00:37
Today we’re talking to my gynecologist Julie Keeler. Julie has been a provider of women’s health care for over three decades. She’s originally from Washington state, where she earned her Bachelor of Science degree in nursing for 13 years following her graduation, she worked as a registered nurse in labor and delivery while still living in Southern California. She also had the opportunity to receive her nurse practitioner education and earn a master’s degree in nursing in 1996. Julie relocated with her family to the Raleigh area and worked initially as a clinical nurse specialist and then in private practice as a nurse practitioner providing obstetric and gynecologic care. Sherry I got through that work in early 2005. Julie has a good fortune to start a local women’s health care practice which has had wonderful success. That’s where I met Julie. Julie also has two terrific adult children shared in price when she has time Julie enjoys the mountains, the beaches, quilting, landscaping, her dogs, chickens, and kayaking.
Cheri Gregory 01:41
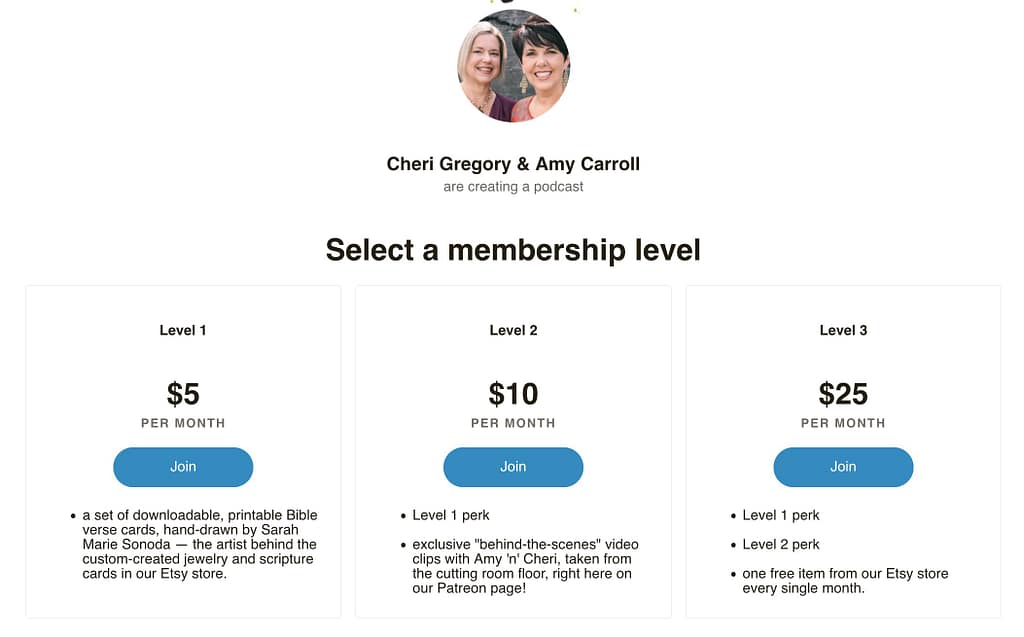
Now most episodes of grit and grace the podcast are sponsored by an author or a publisher. But this interview today was made possible by our faithful Patreon supporters.
Amy Carroll 01:53
Patreon is a service that allows content consumers friends like you to financially support the content that they love sharing I use Patreon funds to pay for things like our graphic designers fees or editors time and subscriptions to the place where grit and grace is stored and distributed.
Cheri Gregory 02:10
We love Love, love staying in touch with our Patreon supporters by sending videos of behind the scenes little snippets from the cutting room floor and usually those involve me throwing me under the bus just for fun.
Amy Carroll 02:24
Ah, yes, they do. And you’ll get to see us with shower and bed head just sayin. So that’s silliness. Let’s dive into today’s interview with Julie
Julie Keeler 02:36
kormos run a lot of our body whether it’s from thyroid, adrenal glands, if it’s up to Jared gland, your ovaries, all of those are endocrine glands. And they talk to each other biochemically through their hormone production. And they’re so cool. Early on in being a nurse and a nurse practitioner. I hated endocrine, I thought this is impossible to figure out. Just don’t ask me about endocrine. And then I realized that my specialty was indicated. I’m like, oh, okay, so I really made friends with that whole concept of the endocrine system as a whole. And they’re all interacting inside your body. And they’re all basically glands of type. And they all talk to each other. They’re best friends. They’re like high school girls. And when one of them goes bad, the other one can follow. And some of them are just along for the ride and get caught skipping school. So I use all that kind of stuff when I talk to patients because if you can see it, you can say Oh, that makes sense. So really being very practical in your illustrations and making the whole process practical and not scary. There are some mystical parts. I mean, have you ever imagined how complex this whole thing is?
Amy Carroll 03:46
It just is right. So Julie, I’m gonna interrupt you because this is already so good. I think we’ve already started. Let me tell everybody though, that is listening today that this is Julie Keeler. She is a nurse practitioner in Holly Springs, North Carolina. And she’s my guy. No. Hey, Joey.
Julie Keeler 04:05
Hey, how are you?
Amy Carroll 04:07
I know you guys are listening to her explain things to me. And now you understand why every woman in Holly Springs goes to Julie. Except that, Julie, I got a letter from you recently.
Julie Keeler 04:19
Yeah, I know, Amy, I’m sorry.
Amy Carroll 04:22
Oh, gosh, I’m so sad. And every woman at Holly Springs, we’re gonna have to have like a kind of figure to funeral because you are moving on to other things. And it’s educating what you’re going to do with us today. So give us in a nutshell what you’re gonna do when you leave me.
Julie Keeler 04:37
Well, I just finished my resume. How’s that? Oh, and I’m 20 years I’ve never needed a resume. And I’m like, Oh, I probably need to write some of this down. And my resume is so simple. I just haven’t skipped around a lot. And I didn’t get into a lot of flowery details. But the reality is, is now that I’ve written it, I need to actually send it to someone. My hope is to teach at the university level
Amy Carroll 04:59
for a year. Ordinary in your field. I think because you’re a nurse practitioner with your own practice, you built your own practice. And I think that one of the reasons that women love going to you, Julie is because you are at heart an educator, you spend far more time with your patients than anyone I’ve ever known because you talk to us about what’s going on with us. And that’s why I wanted to have you answer questions about menopause because menopause, why don’t we talk about this stuff. So just any opening thoughts on menopause in general Julie?
Julie Keeler 05:32
Well, menopause is natural, and it’s normal. And it’s actually rather freeing. When women look back, they say, wow, this is a whole nother stage of my life that I thought I didn’t want to have happen. And then I realized, this actually, is okay, I see our life in lots of stages. But if we’re looking at reproductive health, we have pre puberty when our ovaries are very quiet than our bodies get to a certain body mass and fat content and a certain age and maturity. And then puberty starts. And so once puberty starts, and the ovaries actually wake up and start doing their job, then you’re now in your fertile reproductive years, you go from that up until you get into your late 40s and early 50s. And then our ovaries say, well, I’ve done my job, it is no longer wise for you to bear children. And at that point, our body knows and the ovaries say, you know, peace, I’m out. They’ll sputter a little bit along the way. But your body really is ready for this, it knows it. And then you’re in like the third stage of your reproductive life, and you’re no longer reproductive, but you’re still a powerful woman. There’s lots going on. And that process is I think, what’s kind of scary for women. And we’re famous at this, we do this when women are pregnant, we walk up to them and say, Oh, you’re pregnant. What do you do? And let’s just keep our hands off a stranger’s bellies. I just want to briefly tell her what, please don’t touch humans, pregnant bellies and series freezer section. But the reality is, is that we tell each other these horror stories, and it’s pretty overwhelming. So you enter into your 40s. And you think, Oh, my, When is that going to happen to me? And am I going to lose my mind? And who is going to survive this whole thing?
Amy Carroll 07:09
So in a positive, natural, that’s so good. That’s so reassuring. So we’re gonna dive in our listener sent us a lot of good questions.
Cheri Gregory 07:17
I’d like to pose a question first, though, because I love the description you started out with in terms of the whole system. And I’m wondering if you would walk us through my recent trip through menopause, because I have no idea what just happened to me over the last few years. Like I don’t know what any of those words mean that you said, and I come from a medical family. So just to be clear, that you know, I was as regular as could be every 28 days. And I’ve now gone two years without a period. Don’t be jealous
Amy Carroll 07:44
that brag and so jealous, any of our friends listening, don’t
Cheri Gregory 07:47
be jealous of me,
Julie Keeler 07:48
don’t be bragging about this.
Cheri Gregory 07:50
I was literally soaking in my sweat all night long. And I’m now to the point where I’ll have a little power surge. But within 60 seconds, I’m back to a normal temperatures. So I feel like I’m kind of doing that little tapering down. So just in terms of those high school girls, you talked about, could you just walk us through what just happened to me? Because honestly, I have no idea.
Julie Keeler 08:10
Absolutely. The reality is, is basically your ovaries ran out of eggs, and there’s a predetermined amount of quality genetic material, and it degrades over time. It’s kind of interesting because men make new sperm continuously, right. So there’s the quality of the genetic material. And that part of the union is actually pretty terrific. But with women, we’re born with a number of eggs that we’re going to utilize. And the interesting thing is we’re born with a certain number of by the time we hit puberty, we have like half of them. So there’s all this really interesting process of what goes on in the ovary is complex. The ovaries then work together every month, one of them says, okay, it’s my turn, and it releases an egg and then the other side releases an egg. If you only have one ovary, weirdly enough, that ovary kicks in and says, Okay, I’m in charge now and releases an egg every month, when we get much older into our 40s. Even though we’re still having menstrual cycles, the ovarian quality, or the egg quality is really much lower. And that’s when we start having risks for abnormalities in our pregnancies. And those dramatically go up as we’re in our 40s. So the quality of the genetic material is just not great. And your body knows it. I marvel at it and I’ve done this job for over four decades. And every once while I sit back in an exam room with a patient and I have to stop and say okay, so this is really cool. And it amazes me still how complex yet how simple the process says ovaries basically give off our estrogen and progesterone throughout the monthly ovarian cycle, and it tells the uterus what to do. So really the ovary is in charge the uterus, the uterus simply does what it’s told. So when the ovaries are kind of done, well, they’re kind of done and ovary will no longer be doing ovulation on a regular basis. So you might not populate for six weeks, and then you’ll be late and two weeks later, you’ll have a period So it’s very clear that occupation drives a menstrual period if no conception occurs in that 14 days. And so that’s a whole nother conversation on love. The ovarian cycle is so great. So weird.
Amy Carroll 10:13
You’re such a medical professional, generally.
Julie Keeler 10:19
It’s geeky and geeky. But the reality is, is the ovaries in charge of what the uterus does, and uterus really tries to behave and bleed when it’s told. Now you enter into this perimenopause of time, which is simply your body adjusting to decreased fertility. And there’s a lot of quirky things that start to happen. You Sherry started having a few irregular periods. And then was it a year, two years? Was it six months? Did you skip a period two or three times? And you were done? How did that part go?
Cheri Gregory 10:45
I think I skipped a few months had one skipped a few months had one and then that was it. I didn’t even have breakthrough bleeding. It was just done.
Julie Keeler 10:53
Yeah, that’s awesome, to be honest. And sometimes you think, Well, actually, I kind of hit a concrete wall at that point. And so I don’t know what is better. It just is what it is to go through this irregular bleeding for two years, or to go through six months and be done. And then there’s the concrete wall. And that’s basically the ovaries when they’re not producing an egg stop producing the estrogen and progesterone that drive our reproductive body. And when that happens, all sorts of other things happen as a result. And so you’re lower, you’re low in estrogen, you’re low and progesterone, your testosterone drops also. And those are the three most powerful female hormones. And yes, testosterone is actually a female hormone in smaller amounts than our male counterparts. If we had our male counterpart amount, well, we’d be kind of guy ish. I don’t know how better to say that. And so your ovaries have said, Hey, everybody, I’m done. hormone levels drop, and you’d have symptoms, one of the first symptoms maybe even before you actually miss periods, significantly, his sleep disturbances. I learned that 26 years ago, sitting in a classroom at Cal State in Los Angeles, and I sat there and I was one of 12. And I remember the teacher saying that and I’m like, well, Holy smokes, that’s some crazy stuff. And really, I thought, Okay, this is something very important to women to understand, because we’re all worried about the perimenopause. And we’re really focusing on our menstrual periods, and they’re very important. But even before that happens, we find that there are significant changes and things that are happening around us, it may be mood, it may be irritability, it might be a really close to the surface and grid responses. It may be weeping Enos and more cheerfulness. These are all normal responses to very significant hormones, but sleep disturbances waking up at three or four in the morning, for no good reason. And you are not just groggy, you’re awake. Yeah. And then of course, I say this every day to patients. Yes. And once you’re awake, you solve world peace, don’t you?
Amy Carroll 12:47
Sherry, and I say we have the 2:47am Club. Absolutely.
Julie Keeler 12:51
And that is, I think, primarily menopause or hormone related. Now, granted, there are other things that can cause that. So it can get to be a bad habit. And we’ve only disturbed our own sleep. And we can’t get past that until we actively work on our sleep hygiene is what we call it. But to be honest, if you’re in your mid 40s, or early 50s, and you’re still having periods, but your sleep is really interrupted. It’s probably hormones. Yeah, so that’s really a really important indicator. So when you’re not sleeping great, you’re not doing great. So even if you’re still having your periods and let’s say you’re 49 you should bring this to your providers attention, don’t ignore the facts. think, Oh, well, I had a cook with dinner, or my husband snores or it was too hot in the room. All of those are factors. But if you’re in this perimenopausal age group, and you’re in your 40s, inching closer to your 50s, sleep disturbances are super important. And you need to bring that to your attention of your provider.
Amy Carroll 13:43
So good. You’ve just addressed one I don’t think that was on our list that has been huge for both Sherry and I. And so thank you for addressing that and encouraging women to get some help. Oh, yeah. So we’ll go we’re just gonna run down a little list and let you address things that all of us are concerned about. So the first one of course, of course, is weight gain and our friend Kendra said, for real, is there anything I can do to get rid of this perimenopausal weight gain or now that I’m in film at a pause? Is it for keeps Be honest if this is the new me because it’s been the past five or six years I want to embrace it but if it’s not destiny, what should I do? And then Glenda, this was funny, Julie, cuz, you know, you see my scale. So you know, this was kind of it for me too. I was fine. One day woke up. The next day I walked there it was
Julie Keeler 14:31
there it was, I was losing over the waistline of my jeans. Exactly. And why does this brown not fit? And you’re just losing out of your clothes. You’re like, Okay, I’m voluptuous, but I don’t like it.
Amy Carroll 14:43
But if we want to get back at our jeans, what do we do it?
Julie Keeler 14:46
Can we do anything? This is absolutely one of the most common American woman issues and I live in this culture. I can’t speak to the international cultures and how the women look at their menopause or their weight but in American women It’s a huge big deal. And so different things happen around the same time as menopause. And sure, I do think we can blame menopause for some of our weight gain. I do. And I have a funny theory, I have no science to substantiate it, I’ll share that in a minute. So the reality is, is that our metabolism is also slowing down. And so we have to give credit to the maturing process that our body is in, we’re not 25, we’re not 35. And we’re probably not 45 at this point, and you hit that 50 year mark, and everything goes crazy with your cycles, and you enter into this whole kind of tumultuous, perfect storm of aging and menopause. And so the weight can be absolutely related to the hormonal changes, we also slow down a little bit. And we also maybe, are really busy with professional goals. It’s an interesting time, what’s happening with our family, what’s happening with our profession, what’s happening with our energy level at this time, and how does that influence how physically active I am and what I eat? I’d like to say, Oh, yeah, it’s really easy. It’s like calories in calories out. And I could be really cold hearted and say that, but I’m not really sure it’s that simple. I do like to start from that basis. And if we’re not physically actively using our machine, then we’re not doing as much as we can. So exercise burning calories, using our machine effectively and safely is important. And then taking a look at what we eat, how much we eat. And if you sit down with a nutritionist, they’re gonna say half of your dinner plate should be salad, or fresh veggies, a quarter of it should be your source of protein as lean as you can tolerate. And the other quarter can be your carbohydrate or side dish, I asked my patients to get a ramekin and our little bowl and put that on the plate and put your starches there. So yeah, sometimes it is, Well, you know what, I’m not eating great, or we take out a lot, or my portions are a little bit or I do get second. Sometimes it’s alcohol and alcohols packed with calories. And sometimes just like, well, I just have a glass of wine when I’m making dinner. And if you start to really look at the big picture, maybe it’s a little more than that. Or maybe you don’t drink at all, but alcohol for any of the individuals that are asking questions, we really need to watch our alcohol content, because it’s loaded with calories, late night eating subproblem carbohydrates should be limited. And that’s the best way that we can handle our diet, but it could be permanent. Ladies, if we don’t kind of stay on task, you have to exercise you have to eat healthy, and you have to trust your body. And what you’re left with is really what it is. And I recommend highly that there is a there’s some grace that comes with that we have to accept our bodies. And I think it’s really important because we’ve spent a lot of our American life is women disrespecting our body thinking we’re not perfect girl down the street is perfect. The girl who grows up in high school is perfect that other mom who just had four kids and wears the size eight jeans is perfect. And it’s not right. It’s a real problem, I believe. So we have to be graceful in many ways. And I would like us to consider actually being thankful. And I also have a theory. Now I’ll tell you my little theory, and we can move on. But I have a theory that we’re meant to be curvier after menopause, because our bones stay stronger if we bear weight, and if we’re burying our own weight that counts. Wow. And I really do believe it. I think our body actually is way wiser than we’re giving it
Cheri Gregory 18:08
credit for. And I think it’s normal. So strength is more important than weight.
Julie Keeler 18:12
I really think strength is very important. And I think that wearing clothes that are comfortable and not trying to fit into the size eight jeans anymore, because that’s degrading to yourself. It’s horrible. Why do we beat ourselves up that way?
Cheri Gregory 18:23
Well, thank you so much.
Julie Keeler 18:24
You’re welcome.
Cheri Gregory 18:25
I appreciate that so much. All right. So our next question, I’m just going to give a little bit of a disclaimer to our friends who are listening. But if you have young ears around, you might want to pause the podcast and put on earbuds or come back and listen when there’s nobody else listening. Because the next few questions have to do with and I’ll just leave the names off. But I’m sure there are many of our friends who are listening who are interested in what kind of help can you offer for menopausal depression and lack of libido and then one other person added in and dryness.
Julie Keeler 18:58
And those are all very, very important. We don’t stop having sex because we’re menopausal. But in the long run, we may kind of want to because it’s not on our list for this year. And let me look at my list for January. Oh, there isn’t any sex on their lips. So it is a big concern for women. Also vaginal dryness of sex hurts, it’s not an enticing thing. So if we didn’t want it to start with, and then once we’re getting going and the moisture isn’t there, and you’re like, I feel like I’m being loved with sandpaper or tearing then that’s a very distracting, uncomfortable situation. And I feel strongly that sex needs to be comfortable in order for us to have sex. I don’t think it’s okay to continue to have sex when you’re in pain, don’t you think that’s the wrong message? And so we have to think a little bit more openly about that. And so I think we need to really look at what we can do what we can do in our relationship with our spouse, open communication. I think your spouse needs to kind of know what you’re thinking they may not agree with that. But you could say, look, I need to interject, if your partner is having sex with you, then usually your partner gets to feeling like there’s something wrong with them, or you don’t love them. There’s many ways to be intimate. So I shouldn’t take just sex. But I should say, if the intimacy isn’t there, then your partner is probably going to feel rejected. So even though your sex drive is not high, I think there’s a lot of ways to show that intimacy and that love. And sure, there may be periodically sex. So we will go to Okay, what do we do if I know I should have sex? It’s not a real big drive for me. But now what do we do? So just keeping intimacy alive in your relationship is super important. And that’s not always easy. Sometimes there’s college age or high school aged kids in your household, and they’re up all hours of the night. There’s no privacy.
Amy Carroll 20:44
That was the worst. Yeah. Empty Nest is better hold on girls.
Julie Keeler 20:49
Yeah. How many times have you heard the door knob start to wiggle and you’re like, oh, my goodness, did you really, really super sensitive to it. So it’s hard sometimes to find privacy. And then the business of your world, you get to this age, and you’re usually involved with your family, you also might be a professional, there are demands from your elderly side to the family. So you’re really are that sandwich generation. So you’re very, very tired, you’re exhausted, you’re used up. And when it comes to intimacy, I recommend you actually kind of make time for it in your head, you don’t necessarily tell your partner that every Wednesday you’re going to have sex. I know that sounds really dope. But hey, it’s better than not having sex at all right? When you kind of prepare your own mind, you can decide what Wednesday is going to look like and how you can prepare to have more energy to focus on that. And if it’s twice a weekend, your husband’s going to think he went to heaven. So plan on sex, even if your drive is not telling you to do that, then there’s the other side is sex uncomfortable? Well, we have to do something about that. If sex hurts, then you should not feel that you need to have sex that’s painful. You shouldn’t be thinking, Oh, man, this is not going to feel good, right? So I’m all about lubricants. And I’m all about experimenting, you need to have a good lubricant. It’s okay, your vagina is just not as moist because your hormone level is down. Estrogen is directly responsible for that. And actually progesterone is to some degree when you’re ovulating. So moisture is really, really excellent thing to have around. Don’t feel weird about it, put some on you some on your partner and say, Okay, we’re good to go. It’s a much better outcome and your comfort level and your sensation is going to be better, you won’t be focusing on how bad this hurts. You’ll be saying this is comfortable. And actually the sensation is better over the counter products. Great experiment with what you have heard about. There’s all sorts of them out there. I actually think that coconut oil in the crystal aisle is one of the very best things you can use. And I know that’s kind of against what y’all hear is that oh, I need to use a water based lubricant. But Coconut oil is the King. It’s great. It’s great for your hair is great to cook with. It’s good for your skin. Right? Well
Amy Carroll 22:53
keeps up beside your bed. Absolutely. So
Julie Keeler 22:55
you take and you have your own container by your bed. And yeah, it’s like this. Yeah, yeah, you don’t need to go to the pantry before you have sex.
23:09
I’m looking at you and You’re blushing. That’s hysterical.
Julie Keeler 23:15
reality. And with coconut oil, it doesn’t take very much, but put some on your partner first and then put a small amount at the bachelor and traders The cool thing is, is that it’s fun at room temperature and it melts when it hits your skin so you don’t have this goopy stuff. I know this is very graphic. But the reality is, if you’re annoyed by the messiness, go ahead and use coconut oil and it’s terrific. In fact, I tell menopausal women that if they’re having external dryness, even during their daily activities, go ahead after your shower, just get a little pearl sized amount of coconut oil melted on your fingertips and just put it in those little soft folds. And you’re going to have a more comfortable day. So don’t be afraid to experiment with that. And you’ll find something that you actually think is the best.
Amy Carroll 23:55
Okay, so now we’re gonna move on to the emotional part. And this is something that so many of us struggle with. So what are the ways that we can handle those intense mood swings that can come with perimenopause and menopause. And you know, so many of us feel out of control, and that’s uncomfortable. So what can we do about that
Julie Keeler 24:15
this is essential because it has directly related to your self esteem. And it’s directly related to your productivity of your daily life. And you don’t want to be going to bed every night thinking that you’re a bad mom, a bad sister, a bad wife, a bad daughter, a bad co worker, it affects our esteem deeply. We feel misunderstood, and yet we lash out when something hits us wrong, and it can be cheerfulness and just breaking into crying in the middle of the kitchen because the pot boiled over or the dog walked through the room or your husband didn’t take his shoes off or your kid’s hair isn’t combed. I mean it really doesn’t take much and you just said I’ve had it and that is exquisitely common. So first thing is Be kind to yourself, have grace recognize that you are not alone. And this is something I talked about with Patient today, it’s like everybody thinks that what they’re seeing everybody else is perfection. And it’s just a facade, because when they’re home that night, it’s happening at their home because they’re just people. And some people are really, you know, they’re just like forever a Pollyanna and nothing fazes them. But that’s extraordinarily uncommon, I would encourage each one of us that those mood changes are really, really common, and they can affect your self esteem. But if we can be graceful and forgiving to ourselves, and first step, it’s normal. It’s common, and being respectful to yourself, so that we can maintain a better self esteem, making sure that your family knows, I’m sure they do, you just haven’t talked with him about it. And it’s not your normal you, you don’t recognize you when you’re like that. So things that can help is self awareness, having solitude or personal time. And I think solitude is really important. Some people are afraid to be alone, like they’re gonna be lonely. And I would encourage us to make friends with solitude so that we can be with ourselves. I think that’s super important. I think being mindful, being in the moment, and we are famous as American women, as being multitaskers. We’re actually taught that that’s our job. I think, exercise enough sleep is essential, and the menopause creates poor sleep. So we’re like, well, we’re kind of darned if we do. And darned if we don’t, we must get good sleep. And if we can do that naturally, great. There’s all sorts of different interventions. And there are also some pretty innocent sleep aids that can help you get through the menopausal sleep issues. And you should talk to your provider about those. Julie, do
Amy Carroll 26:33
you think there’s a time to see a counselor during this time? And what does that look like?
Julie Keeler 26:38
I think it’s a very important part of maintaining your self esteem and helping you understand that you’re out of character, but you’re not out of your mind. This is very, very strong hormones that are fluctuating, and it’s creating hormonal shifts in your brain also. And we have to be really respectful of that. So yes, I think a counselor is an excellent plan. And I think that getting a good counselor that understands women is super important. And you kind of have to kind of search for that you have to look around, you have to do your research, you have to ask your friends, you have to take a look at reviews. And it should be someone who really doesn’t mind sitting and talking to a menopausal woman. And also, if your gynecologist is not open to discussing this with you, you need a new gun ecologist, some primary care providers are great, you may have a great nurse practitioner at your primary care that you see, or a PA or even an MD that says, Yeah, we’re going to take this half hour, and we’re gonna we’re gonna sit down together about this. And so you need to have someone who actually understands and respects the menopausal shift, because it’s complex, and you need to feel heard, you need to feel listened to.
Cheri Gregory 27:43
So can you talk just a little bit about this whole concept of keeping hormones in balance are there like I didn’t take anything I didn’t see my my doctor or anything. It just I did this all by myself. So. So are there safe hormones to take for hot flashes? Or are there natural remedies talk to us about hormones, on hormones balance, and anything that we could do for hot flashes?
Julie Keeler 28:09
Oh, of course. Well, I think there are some options available and some women don’t need anything. They just are the she Wolf, and they just carry on and you were a she wolf? Didn’t mean to be. Yeah, well, you’re probably wicked busy. And you thought okay, well, this will be okay. And you just next thing you know, two years later, you’ve made incredible progress. But the reality is, is that there are hormones that can be used. If your family or personal health history counter indicates the use of hormones at menopause, then we need to be open to what other options are available. So those kind of contraindications include a history of stroke, uncontrolled high blood pressure, abnormal vaginal bleeding, that we don’t know why the history of breast cancer in yourself a history of inherited breast cancer risk, multiple individuals in your family that have breast cancer or ovarian cancer, those questions or those family histories would lead us to having a conversation and maybe getting tested to see if we are at risk for those cancers. The American College of ob gyn recommends that if you do choose to give hormones to patients that you should use the lowest dose that works for the end that fully treat the symptoms, and that you should use it for five years or less. But they also say that there are going to be some outliers. So hormone replacement therapy is not wrong. It’s acceptable in the right situation and the right patient for difficult symptoms. My recommendation is have a have a straightforward conversation about about it with your provider, make sure you don’t have counter indications. And if you are moderately or severely affected by these menopausal issues, then we should do something about it. And eventually, two years, five years, seven years will weighing you down and wean you off and it will be okay. But the reality is right now we have to help and if hormones are acceptable, I highly recommend you have that conversation now. If you can’t take hormones, or you don’t want to take hormones, or you’re afraid of them, and your hot flashes in your sleep are really, really bad or your mood, then we should be taking a look at some of the medications that are out there that can help with that the medication effects are is really well known to help with hot flashes, it is an anti depressant, but it really kind of helps with hot flashes, I would actually challenge that I think most antidepressants actually probably helped some with hot flashes, but effects are is kind of well known for that in our specialty. So if there’s no contraindications to use an antidepressant, then that could definitely help with hot flashes. But the patient doesn’t want to take prescription level of estrogen. There are some over the counter products that are very mild and that I know I’m not against use of them. So there’s one called bruh feminine, and I’m just giving name brands so you can look for them. And you can use storebrand. But there’s about three or four of them out there. And they have plant estrogen in them. And it’s it’s a very modest amount. And if you can take that product and if you sleep better or your hot flashes are better, and it’s manageable at that point, and you’re happy with your choice. I think that’s okay,
31:05
great.
Amy Carroll 31:06
So Julie, tell us one last thing if you had one piece of encouragement to give women that are facing menopause or in menopause, what would you tell them
31:15
you are going to be okay?
31:19
Yeah,
Julie Keeler 31:20
you are going to be fine. Get a provider that hears you know what your options are, take good care of yourself. Use medications if you need to, it’s only temporary and in the end, you can be okay.
Cheri Gregory 31:33
We hope you’ve enjoyed Episode Number 213 of grit and grace the podcast
Amy Carroll 31:39
and we want to say thank you to our amazing band of Patreon supporters who made this episode and many others possible for you. Check out our webpage at grit and grace the podcast.com slash Episode 213 there you’ll find the transcript and a link to the grit and grace Patreon page. If you’re not yet a member of our Facebook group, we would love to have you join us just go to Facebook, search for grit and grace the community and you’ll find us next week we’ll be talking with Barb roost authored have surrendered 40 devotions to help you let go and live like Jesus
Cheri Gregory 32:14
for today. Grow Your grit,
Amy Carroll 32:17
embrace God’s grace.
Cheri Gregory 32:19
And as God reveals the next step to live your one life. Well
Amy Carroll 32:22
we’ll be cheering you on. So take it
You’ll never miss an episode when you sign up for weekly updates!